Ruminating on Results
I'm half way through my treatment and have recently received my CT scan which shows just how well the treatment is working... but for some reason I don't seem to be able to pop the champagne...
This month I had my last Obi infusion (cycle 6 out of 12) which means I’m now half way through my treatment trial! From now on, all I have to do is take my daily Venetoclax pills and attend regular appointments with my specialist. There’ll be another CT scan at about Cycle 10 and a bone marrow biopsy after the 12 Cycles, looking for undetectable Minimal Residual Disease (MRD).
Leaving the Cancer Clinic infusion room was filled with mixed emotions for me. It’s become a haven of sorts. A quiet respite in an otherwise full life as a working mum.
In my chair, I’ve been the subject of tender care, attention to my needs and a place focused on keeping me alive. The Obinutuzmab infusions literally dropped my cancer count to almost nothing in my first few days of treatment. Along with my trial nurse, they have been my ally and friend. In some ways they have come to represent safety, security, life.

I know I still have another 6 months of Venetoclax ahead of me, and that too will keep those cancer cells right down… but I can’t help but wonder, “what then”? The complexity with CLL, is right now there is no medical cure. There are amazing treatments that buy time, sometimes a good many years, but inevitably, it is expected that at some stage the cancer will return, again and again until it gets the better of me (sorry, not trying to be depressing, just pragmatic). And I’ve found it difficult to celebrate my results, my response, while this shadow lingers.
THAT question
People often ask “how is treatment going?” and it’s a well meaning question, born out of concern and care but, recently, I’ve found myself rapidly trying to deflect and defer away from their focus on me. I’ve become adept at maneuvering the conversation around to them and their lives. Deftly dodging and diving around the issue. That question seems to suck the life out of me.
But when I’m at home alone, I ponder “why?” Why do I wince and withdraw every time that question comes up?
Mid-term Results
So firstly, because it is the question on everyone’s lips, let me answer it; let me share my half-way results with you, and then I’ll try and unpack my rumination on my reluctance to talk about them…
In simple terms, there are a number of ways we will know if the treatment has been successful…
My white blood cell and lymphocyte count reduce to normal levels
The trial has identified and is monitoring 6 target lymph nodes to see if they reduce back to normal size
Other non-target organs and nodes reduce to normal size
I achieve an undetectable level of Minimal Residual Disease in my bone marrow
My Specialists Reassurance
Today, as my specialist ran me through my results, he came across genuinely pleased, reassuring and positive… saying that by all accounts, my body as responded really well to the treatment and, from the blood tests and physical examination, he’d consider me close to achieving a “complete clinical response.” Which is awesome and uplifting news!
Let’s take a look at what’s led him to that conclusion…
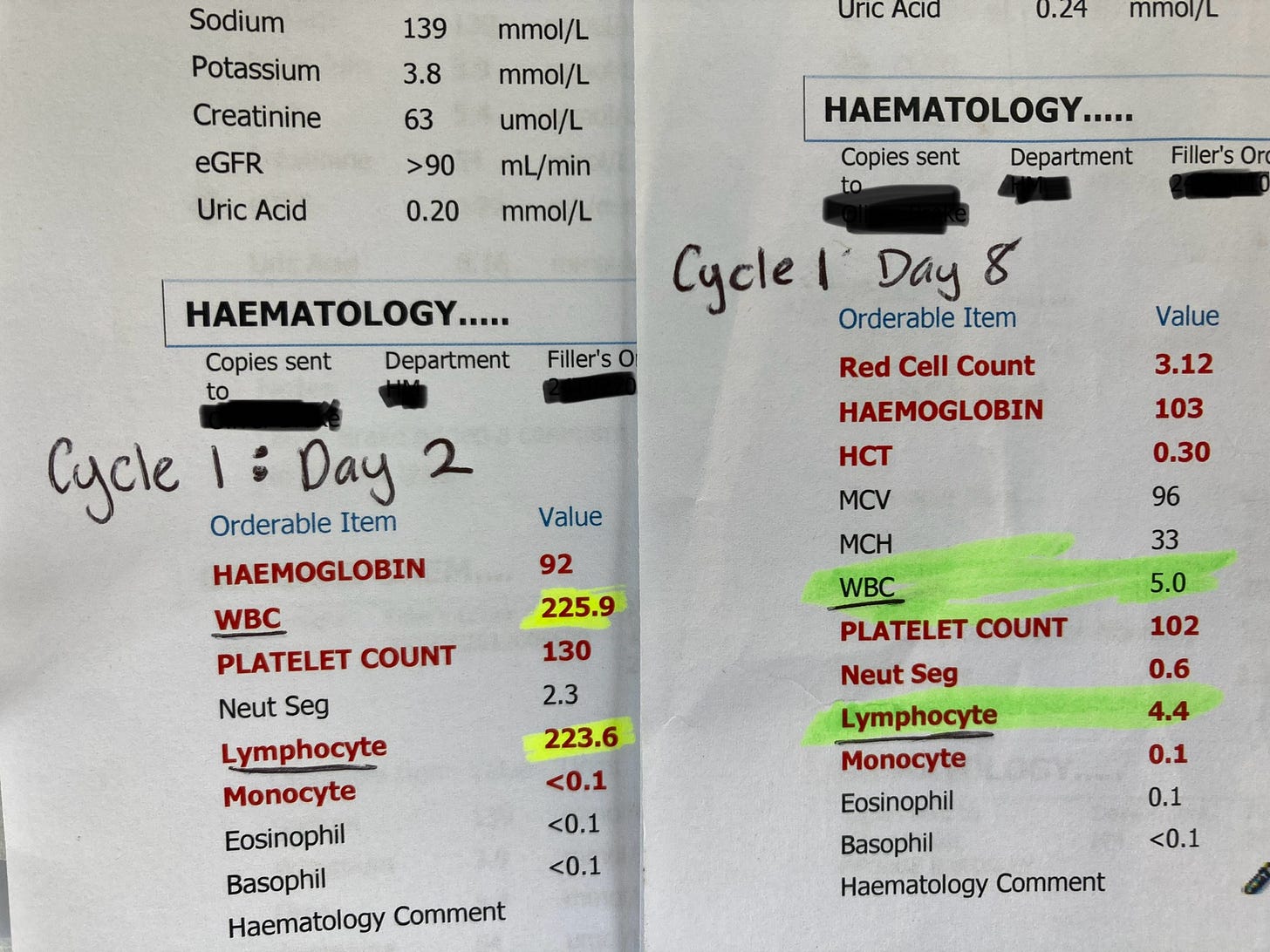
Cancer Cells in My Blood
Very early on in the treatment my WBC and Lymphocyte counts reduced to normal and often below normal levels of cells. It was a rapid reduction of lymphocytes - from pre-trial high of 330.4 to 223.6 after the first day and then, only a week later, down to 4.4! Totally remarkable and exhilarating and very much a highlight of the treatment journey so far.
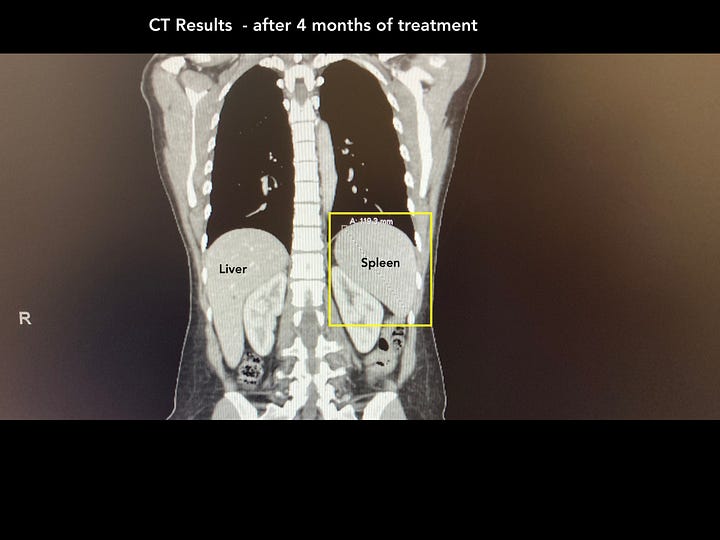
Six target lymph nodes
At my second CT scan the 6 target lymph nodes were measured against my baseline sizes. Over the first four months they have reduced by 79.9% and all but one has reduced to within the normal size range (>15mm). The one stubborn node is lingering just above the acceptable cut off at 17mm. Only being 2mm above the nominal cut off, it could mean any number of things, from just being a slightly bigger node, to it fighting something the day of the CT scan, to (the unlikely event of) residual cancer cells hiding… and based on the positivity of my specialist, it’s not something to worry about.
Other non-target organs
The result I’ve been most amazed by is my spleen. It got very enlarged prior to treatment… as you can see in the photo below… and has now reduced back down to normal. Seeing the photos on my specialists screen really brought home just how unwell my insides were when I started treatment - I wasn’t feeling that sick or overcome by cancer, I could not see my spleen, although it was palatable on examination but this photo demonstrates just how pervasive the cancer was!

MRD in Bone Marrow
This test will happen further down the track, so in the meantime please pray for my treatment to cause deep, deep undetectable MRD (<10−6) … “as several studies have shown the close correlation of End of Treatment MRD status with Progression Free Surival (PFS) and Overall Survival (OS).5,13-17 The depth of remission should therefore be proportional to the time to disease relapse.2,1” In simple terms, if measurable levels of cancer cells are still detected, remission time will likely be short; if it is really hard to find evidence of cancer cells, a deeply undetectable MRD, my remission time will hopefully be for many years. Undetectable MRD (uMRD) is currently defined as the presence of less than 1 CLL cell in 10,000 leukocytes (<10−4) and it can get as low as (<10−6). Anything between (<10−2-<10−4) is considered an intermediate response and anything higher than (<10−2) is not optimal for long term results/remission.
My Reluctance
Phew, all good news, but so complicated right? On typing all that out, I realise, a part of my reluctance to talk results is simply because it all seems so complex and each aspect of the results comes with so many implications, individually and collectively. Leukemia is, unfortunately, not a tumor they can identify and target with chemo, radiation or surgery. Which is what makes CLL so difficult to find a cure for. And that makes it difficult for me to try and explain it simply. To be honest, I find all the intricacies of it overwhelm me and are not the response people are looking for when they ask that question.
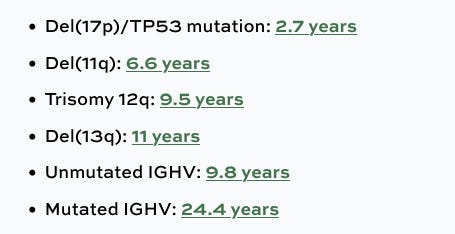
The second reason I find it so hard, is my journey has been anything but textbook (if there even is one!). I’m in a younger demographic (between 5-10% are diagnosed with CLL under 50), I was told CLL was a slow to develop cancer and I didn’t have any of the “high risk” markers (TPH53, IGHV, 17pDel etc), yet in 18months mine sky-rocketed. Without any clear reason or explanation, I found myself already having my first treatment, while others with my genetic markers can go without for 10-20yrs.
Here’s an example of how complex the data is for how long someone can usually live without treatment (from their diagnosis) based on some of the known genetic markers…
(FYI, I’m in the Mutated IGHV group and, according to statistics, could have enjoyed 24yrs before my first treatment. I got 18 months.)
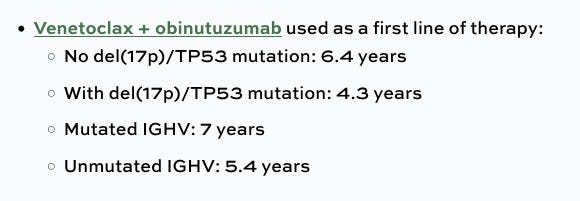
And then here’s some data around the progression free survival time (remission) after Venetoclax and Obinutuzmab treatment…
So technically I could look forward to 7 years ahead with no cancer…but once bitten, twice shy right?
The Bite
And here’s the deeper reality of my reluctance to share and celebrate my results. I’m scared. For 18 months, every blood test has been a shock to my system. I’ve come to live seeing results as a constant and real threat to my existence.

None of my trajectory matches anything I can find in research papers and statistics. I do find the odd person online who has shared a similar journey, but not many. I don’t feel confident in my chances of a lengthy remission, not until I am still living cancer-free in 2030 and there’s a lot of blood tests between now and then. I need my remissions to be long and lasting because I have three kids to raise, but what if they’re not? There is such a significantly monumental unknown to my days ahead and I have no idea what my results mean. My “safe” genetic markers meant nothing in the unusual progression of my illness, so I don’t have much faith that my results alone will predict my length of life from today forwards. Gloomy sound huh? I’m sorry, I think I’m building to something positive… (but while we sit here, if this resonates, this uncomfortable conversation about results and what they really mean, I’ve shared this because I want you to know you are not alone in the wrestling.)
Cancer-free conversations
So my blood tests and CT scans results on the surface may seem positive at this stage in the treatment journey, but my inability to have a full-blown party comes out of a deeper daily awareness that I am mortal (as we all are), and there is no straightforward way, no certainty I can give, no nicely packaged response to that question “how is your treatment going?”
So what can we do about this? My gut feeling is, let’s start by changing up the question. Instead of always asking “how’s treatment going?” or “what’s happening with your treatment?”, what if we asked other questions to people going through cancer or give them permission to not talk about their cancer at all. I have a few good friends who have communicated to me that they know I do not want cancer to define me, that they love and want to hear about who I am away from my silent shadow, that have given me permission not to answer that question and talk about other things that are important to me. And I have lots of other things I’d love to talk about! I don’t know how long I’ve got on this planet, but while I’m here I’m still planning on extracting everything out of my time.
I love to focus on plans and preparations and activities and adventures and family celebrations and magic moments and making memories. Talking about these things are what quiet down the search for a reassurance that I’ll never find on a medical result print out.

I went out to dinner recently with a friend I haven’t seen for ages, and as we sat down, she thoughtfully prefaced our time together with, “I care about you and am happy to talk about your cancer journey, but if you don’t want to, I can be that fun friend where we talk about everything but…” Wow, did that instantly relieve me of the pressure that was building and provide me with permission to talk about so much else that is important to me. I felt very seen and known and loved in that moment. I was very grateful.
The elephant was named, and then sent to bed with a gentle hug.
Courage, Love and Legacy: Points to Ponder
If you’re a cancer patient and, like me, find times when you struggle with the questions of how life with cancer, treatment or remission are going, and agonize over the a constant focus on your condition, your health, your cancer, I’d encourage you to find a gentle way of letting people know you’d rather carry the conversation somewhere else. I’ve started saying “thanks for asking, would you mind if we park that part of my life and talk about the rest of it today?”. I know our friends and family have the best intentions, and sometimes we do want to share and give them an update… and other times we don’t. Because they don’t know, it’s a good idea for us to have the courage to communicate our needs clearly, so they can support us well. What could you say when you need space from your condition? What might you say when you really do need someone to share your heart with?
If you’re a friend, family or part of a community of people supporting someone with cancer, I’d gently encourage you to consider your approach when catching up. It’s important you do show you care about their cancer AND it’s important you care about the other aspects of their lives too. How can you mix it up a bit, giving them permission to talk or not about what’s going on for them in that realm? I know it’s a delicate balance between ignoring a really significant part of their lives (by never asking) or making it the only significant feature of their lives (by asking all the time)… Have a think about ways you can compassionately navigate these conversations with your loved ones…
Here’s to us all growing in courage, love and legacy
Kylie



Thanks Kylie for letting us know what specifically you need prayer for and that you are doing well so far.. I get why you don 't want to have a party just yet. You are coping well with an incredibly difficult condition.
Love Jill